A one-stop clinic for patients with breast issues.
Dr. David Clark established The Breast Centre in 1988 with a vision to provide a “one-stop shop” for patients with breast problems. In 2011, this expanded into a comprehensive breast cancer clinic in new purpose-built rooms, and is now the largest single practice involved in the management of breast cancer in the Hunter.
Did you know?
Our breast surgeons offer their own core biopsies and cancer localisations, which reduces delays to surgery and helps to minimise patient wait times. By performing their own localisation on the day of surgery, our surgeons are able to better plan for the operation and minimise patient discomfort leading up to the procedure.
Being breast aware
Breast problems can affect women and men at any age. They can show up as a result of menstrual periods, pregnancy, lactation and advancing age, and the majority of the time these problems aren’t a cause for concern. Some examples of typically non-cancerous breast changes include breast lumpiness, presence of cysts, breast pain, abscesses and nipple discharge.
However, there are certain risk factors that increase the likelihood of developing breast cancer. Being a woman is the single biggest risk factor, and this risk increases with age. Other factors that can indicate an increased risk are a strong family history and gene mutations. Having certain risk factors doesn’t necessarily mean you will develop breast cancer, and not having risk factors unfortunately doesn’t indicate you won’t be diagnosed with it.
For this reason we encourage women and men of all ages to be breast aware by doing regular self-checks, which are a very effective tool for the early detection and prevention of breast cancer.
How to check your breasts
LOOK
Look at the shape and appearance of your breasts and nipples in the mirror, hands by your sides. Raise your arms above your head and have another look.
FEEL
Feel your breasts and nipples, looking for anything that isn’t normal for you. Feel from your collarbone to below your bra-line, and under your armpit too.
LEARN
Learn what’s normal for you. Breasts come in all different shapes and sizes, so get to know your normal. See your doctor if you notice any changes.
Breast imaging
-
Breast ultrasound uses sound waves to produce highly detailed pictures of the internal structures of the breast, which helps to diagnose breast lumps or other abnormalities found during a physical exam, or on a mammogram or breast MRI. Ultrasound is safe, noninvasive, and doesn’t use radiation, so it’s often used for young, pregnant or breastfeeding women. You will need to undress from the waist up and we will provide you with a gown to wear during the exam. Breast ultrasounds are performed by our skilled sonographers, with results interpreted by a radiologist on the day.
-
Also known as breast tomosynthesis, this is an advanced form of breast imaging that produces 3D images of the breasts using low-dose x-ray and computer reconstructions. In this exam, the breast is compressed between two plates, which helps reduce the amount of radiation needed to penetrate the breast tissue, and produces clearer images by spreading out the breast tissue. The x-ray tube then moves in an arc over the compressed breast, capturing multiple images of each breast from different angles. These 3D image sets help minimise the tissue overlap that can hide cancers or make it difficult to distinguish normal overlapping breast tissue from tumours.
-
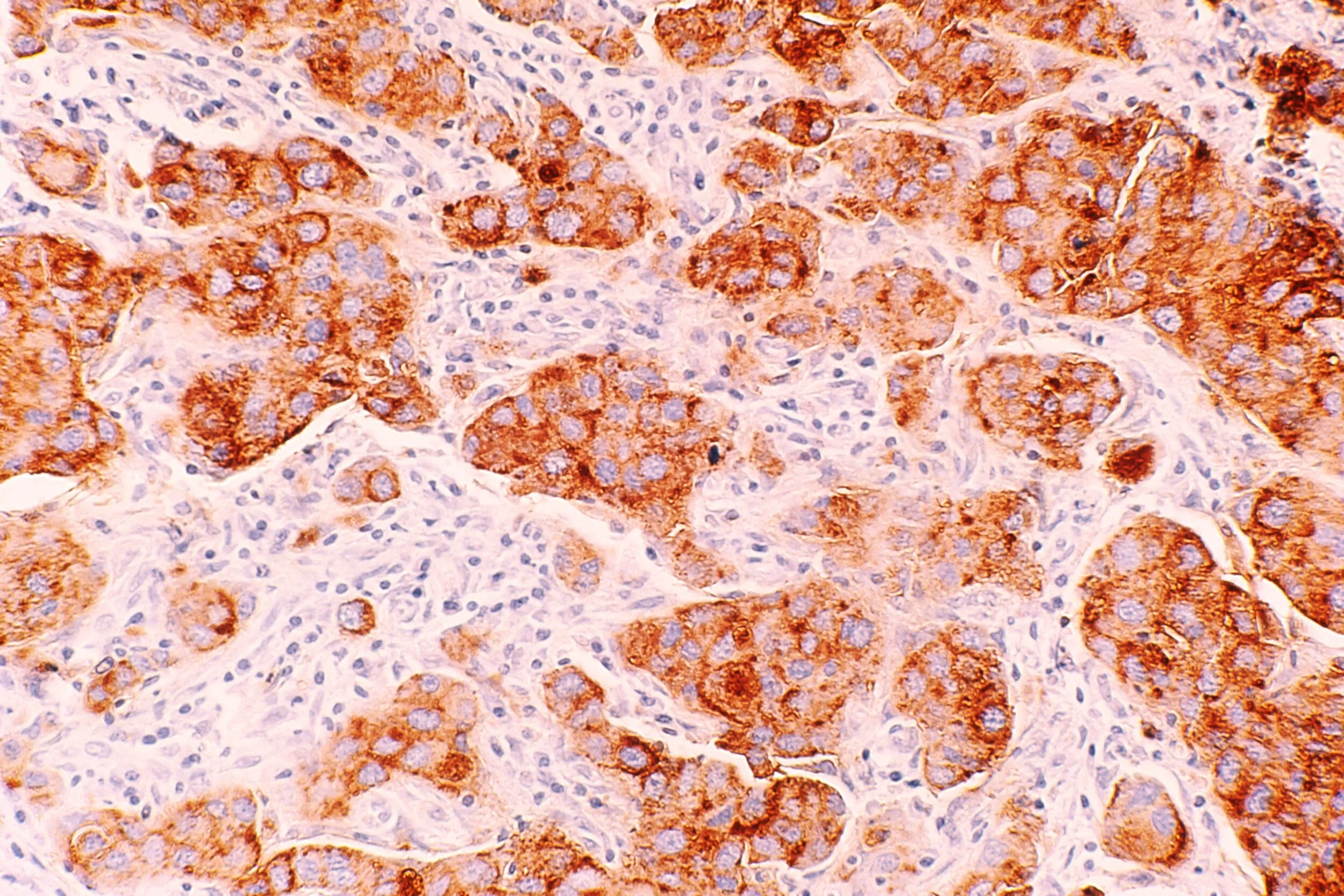
Using ultrasound guidance and local anaesthetic, a breast physician uses a very thin needle to collect a sample of cells from the area of concern. A pathologist analyses this sample on the day and provides a diagnosis, or requests further testing.
-
This type of biopsy was developed as an alternative to surgical biopsy, using mammography to pinpoint and biopsy an abnormality within the breast. It’s a less invasive way to collect the tissue samples needed for diagnosis, requires less recovery time and causes minimal scarring. Local anaesthetic is used, and a tiny marker may be placed in the breast tissue after the procedure to mark the biopsy site for future reference. This sample is sent to a pathology lab to determine if there are cancer cells present.
-
A core biopsy is performed with local anaesthetic and guided by ultrasound, however unlike a fine needle aspiration biopsy, it allows us to collect a larger tissue sample. This sample is sent to a pathology lab to determine if there are cancer cells present.
Our breast doctors use imaging to help with the assessment of breast concerns. If indicated, they will also use fine-needle core biopsy or stereotactic biopsy to collect samples of cells or tissue, which can provide additional information about breast concerns.
Breast surgery
-
The aim of breast-conserving surgery is to remove the cancer while keeping as much of the breast tissue and shape as possible. The cancer is removed, along with some normal-looking tissue around it (known as the margin). This is called a wide local excision. Radiotherapy usually follows breast-conserving surgery, to reduce the risk of the cancer coming back in the breast.
-
A mastectomy is the surgical removal of the entire breast, including all of the breast tissue and sometimes other nearby tissues. There are several different types of mastectomies, including nipple-sparing mastectomy and double mastectomy. Following a mastectomy, some women may choose to have breast reconstruction, or wear an external breast prosthesis.
-
If breast cancer spreads, it typically goes first to nearby lymph nodes under the arm. In lymph node surgery, one or more of the lymph nodes are removed and examined in a lab. Knowing if the cancer has spread to your lymph nodes helps your doctor find the best way to treat your cancer. This surgery can either be done at the same time as your breast cancer removal, or as a separate operation.
-
Breast reconstruction surgery recreates the shape of the breast following a mastectomy or, occasionally, breast-conserving surgery. Depending on your individual circumstances, this can be done at the same time as your surgery, or as a separate procedure at a later time. Some patients may also need to have surgery to their non-affected breast at some point to correct their symmetry.
There are several different types of surgery performed for breast cancer. The type of surgery performed is unique to each patient, depending on their circumstances. The aim of surgery is to remove as much of the cancer as possible, through either breast-conserving surgery or mastectomy. Surgery is also used to examine the nearby axillary lymph nodes under the arm.
Breast therapies
-
Radiation therapy, or radiotherapy, uses a controlled dose of high-energy radiation to kill cancer cells. It’s a localised treatment, which means it generally affects only the area being treated. Radiation therapy is usually recommended for patients who have breast-conserving surgery. It’s also sometimes used following a mastectomy to target any cancer cells that may remain in the chest wall. Each patient’s radiotherapy schedule is different, but it’s typically administered daily (excluding weekends) for three to six months.
-
Chemotherapy, or chemo, is the use of drugs to kill or slow the growth of cancer cells. There are many different types of chemo drugs, and because different drugs work on different types of cancer, the type(s) each patient is prescribed is unique to their cancer. Sometimes chemotherapy is the only treatment needed, but other times it’s used alongside surgery, radiation therapy or other drug therapies. Depending on the type of cancer and the drug being used, chemotherapy can be given orally, through a needle inserted into a vein, or by introducing drugs directly into an organ or tissue affected by cancer as a cream applied to the skin. Each patient’s chemotherapy schedule is different, but it usually consists of a combination of drugs given in a specific number of cycles over a set period of time. It may be given once a week, once every two weeks, once every three weeks, or even once every four weeks over a three to six month period.
-
Hormone therapy, or endocrine therapy, is used to treat cancer that tests positive for either oestrogen or progesterone receptors. This type of cancer uses hormones to fuel its growth. The aim of hormone therapy is to block hormone actions or lower hormone levels in the body to help stop the spread of the cancer. Recent clinical trials have also indicated that hormone therapy can be used to prevent breast cancer in women who are at an increased risk of developing the disease. Each patient’s hormone therapy schedule is different, but patients should usually expect five to 10 years of hormone therapy.
-
Targeted therapy uses medicines to target proteins in breast cancer cells that contribute to cancer growth and survival. These treatments are very focused and work differently than chemotherapy. Targeted therapy can be used to treat HER2-positive cancer, hormone receptor-positive cancer, patients with BRCA gene mutations, and triple-negative breast cancer. Targeted therapy can be given in the vein (IV), as an injection under the skin, or as a pill. Every patient’s targeted therapy schedule is different, but it typically involves doses, or infusions, administered every three weeks, continuing for up to 12 months.
-
Immunotherapy uses medicines to encourage the immune system’s natural ability to recognise and destroy cancer cells. Its use as a breast cancer treatment is currently limited to specific subsets of breast cancer, however clinical trials are underway to expand its use to more breast cancer patients. The most common type of immunotherapy treatment uses drugs known as immune checkpoint inhibitors to restore immune system function. Certain types of breast cancer, such as metastatic triple-negative breast cancer, have been shown to respond well to immunotherapy treatments.
Breast cancer therapies take several different forms. The aim of using therapies prior to surgery (neoadjuvant) is to shrink the size of the cancer, making it easier to remove. Some therapies can be used alongside each other to more effectively remove a cancer. The aim of using therapies after surgery or other therapies (adjuvant) is to remove any remaining cancer cells and help lower the risk of cancer recurrence. Our breast doctors work alongside medical oncologists and radiation oncologists, who are specialists in diagnosing and treating cancer using different therapies.
Breast cancer trials
-
A Phase III, Open-Label, Randomised Study to Assess the Efficacy and Safety of Camizestrant (AZD9833, a Next Generation, Oral Selective Estrogen Receptor Degrader) Versus Standard Endocrine Therapy (Aromatase Inhibitor or Tamoxifen) as Adjuvant Treatment for Patients with ER+/HER2- Early Breast Cancer and an Intermediate-High or High Risk of Recurrence Who Have Completed Definitive Locoregional Treatment and Have No Evidence of Disease
The purpose of CAMBRIA-2 is to find out if giving a new treatment called camizestrant is better at reducing the chance of cancer from coming back compared with the usual endocrine treatments such as letrozole, anastrozole, exemestane or tamoxifen. Camizestrant is a type of endocrine treatment called a ‘selective oestrogen receptor degrader’ (SERD). Camizestrant works by breaking down the oestrogen receptors in cells, and also blocks the oestrogen receptors from being triggered by oestrogen. This prevents ER-positive cancer cells receiving messages to grow and multiply. Camizestrant may help to reduce the chance of cancer coming back. The research will also find out more about the side effects, safety and effectiveness of camizestrant.
-
A Randomised, Double-Blind, Placebo-Controlled, Multi-Center, International Phase 3 Study to determine the Preventive Effect of Denosumab on Breast Cancer in Women carrying a BRCA1 Germline Mutation.
The purpose of this research is to find out whether Denosumab can help prevent breast cancer in women with a BRCA1 mutation. It also aims to find out whether Denosumab decreases the risk of developing ovarian cancer or other types of cancer, study the safety of using Denosumab, and study its effect on bone health.
-
EMBER-4 - A Randomized, Open-Label, Phase 3 Study of Adjuvant Imlunestrant vs Standard Adjuvant Endocrine Therapy in Patients who have Previously Received 2 to 5 years of Adjuvant Endocrine Therapy for ER+, HER2- Early Breast Cancer with an Increased Risk of Recurrence.
Doctors and researchers are trying to find new medicines that could treat estrogen receptor positive (ER+) and human epidermal receptor 2 negative (HER2-), early breast cancer. Clinical research studies like the EMBER-4 study are an important part of this work. The main purpose is to measure how well imlunestrant, the investigational medicine, works compared to standard hormone therapy in participants with early breast cancer that is ER+ and HER2-.
-
A double-blind, placebo controlled, randomized phase III trial of Fulvestrant and Ipatasertib as treatment for advanced HER-2 Negative and Estrogen Receptor positive (ER+) breast cancer following progession on first line CDK 4/6 inhibitor and aromatase inhibitor.
The FINER study is for participants with advanced or metastatic breast cancer that is ER-positive and HER2-negative which has progressed on prior treatment. The primary aim is to determine whether cancer can be controlled for longer in patients treated with ipatasertib (a drug that can slow the growth of cancer) and fulvestrant, compared with those treated with the standard treatment of fulvestrant on its own.
-
A phase IIIb study to characterize the effectiveness and safety of Adjuvant ribociclib in a wide patient population with HR+ HER2− early breast cancer (Adjuvant WIDER).
Adjuvant WIDER is testing a potential new treatment called ribociclib, for participants with hormone receptor positive (HR+) and human epidermal receptor 2 negative (HER2-) early breast cancer. The purpose of the study is to evaluate the safety and efficacy of ribociclib given in combination with standard endocrine (hormonal) therapy to see if ribociclib can help reduce the risk of breast cancer recurrence.
-
Can a web-based psychosocial intervention improve mental quality of life for women with metastatic breast cancer?
This study is aiming to find out whether using the Finding My Way – Advanced program leads to significant improvements in mental quality of life and a decrease in distress for women with metastatic breast cancer (MBC). The program is a six-module online psycho-therapeutic program consisting of video and written personal accounts from women living with MBC, educational videos, self-management activities, audio relaxation and mindfulness tracks, and print information.
-
Optimal Personalised Treatment of early breast cancer using Multi-parameter Analysis.
The OPTIMA trial aims to find out if using a test called Prosigna can help make safe and accurate decisions about whether or not chemotherapy treatment is needed for participants with ER-positive, HER2-negative early breast cancer.
Good outcomes for many people diagnosed with breast cancer today are due to the work achieved by clinical trials, and we’re always working on several important research areas to address patient needs.
Here you can read about the current trials we’re running that are open to recruitment for applicable patients.